Bayesian reasoning implicated in some mental disorders
From within the dark confines of the skull, the brain builds its own version of reality. By weaving together expectations and information gleaned from the senses, the brain creates a story about the outside world. For most of us, the brain is a skilled storyteller, but to spin a sensible yarn, it has to fill in some details itself.
“The brain is a guessing machine, trying at each moment of time to guess what is out there,” says computational neuroscientist Peggy Seriès.
Guesses just slightly off — like mistaking a smile for a smirk — rarely cause harm. But guessing gone seriously awry may play a part in mental illnesses such as schizophrenia, autism and even anxiety disorders, Seriès and other neuroscientists suspect. They say that a mathematical expression known as Bayes’ theorem — which quantifies how prior expectations can be combined with current evidence — may provide novel insights into pernicious mental problems that have so far defied explanation.
Bayes’ theorem “offers a new vocabulary, new tools and a new way to look at things,” says Seriès, of the University of Edinburgh.
Experiments guided by Bayesian math reveal that the guessing process differs in people with some disorders. People with schizophrenia, for instance, can have trouble tying together their expectations with what their senses detect. And people with autism and high anxiety don’t flexibly update their expectations about the world, some lab experiments suggest. That missed step can muddy their decision-making abilities.
Given the complexity of mental disorders such as schizophrenia and autism, it is no surprise that many theories of how the brain works have fallen short, says psychiatrist and neuroscientist Rick Adams of University College London. Current explanations for the disorders are often vague and untestable. Against that frustrating backdrop, Adams sees great promise in a strong mathematical theory, one that can be used to make predictions and actually test them.
“It’s really a step up from the old-style cognitive psychology approach, where you had flowcharts with boxes and labels on them with things like ‘attention’ or ‘reading,’ but nobody having any idea about what was going on in [any] box,” Adams says.
Applying math to mental disorders “is a very young field,” he adds, pointing to Computational Psychiatry, which plans to publish its first issue this summer. “You know a field is young when it gets its first journal.”
A mind for math
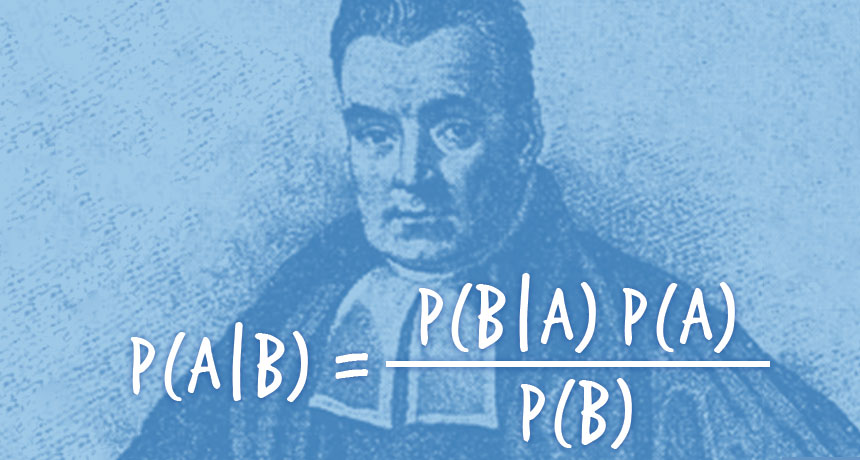
Bayesian reasoning may be new to the mental illness scene, but the math itself has been around for centuries. First described by the Rev. Thomas Bayes in the 18th century, this computational approach truly embraces history: Evidence based on previous experience, known as a “prior,” is essential to arriving at a good answer, Bayes argued. He may have been surprised to see his math meticulously applied to people with mental illness, but the logic holds. To make a solid guess about what’s happening in the world, the brain must not rely just on current input from occasionally unreliable senses. The brain must also use its knowledge about what has happened before. Merging these two streams of information correctly is at the heart of perceiving the world as accurately as possible.
Bayes figured out a way to put numbers to this process. By combining probabilities that come from prior evidence and current observations, Bayes’ formula can be used to calculate an overall estimate of the likelihood that a given suspicion is true. A properly functioning brain seems to do this calculation intuitively, behaving in many cases like a skilled Bayesian statistician, some studies show (SN: 10/8/11, p. 18).
This reckoning requires the brain to give the right amount of weight to prior expectations and current information. Depending on the circumstances, those weights change. When the senses falter, for instance, the brain should lean more heavily on prior expectations. Say the mail carrier comes each day at 4 p.m. On a stormy afternoon when visual cues are bad, we rely less on sight and more on prior knowledge to guess that the late-afternoon noise on the front porch is probably the mail carrier delivering letters. In certain mental illnesses, this flexible balancing act may falter.
People with schizophrenia often suffer from hallucinations and delusions, debilitating symptoms that arise when lines between reality and imagination blur. That confusion can lead to hearing voices that aren’t there and believing things that can’t possibly be true. These departures from reality could arise from differences in how people integrate new evidence with previous beliefs.
There’s evidence for such distorted calculations. People with schizophrenia don’t fall for certain visual illusions that trick most people, for instance. When shown a picture of the inside of a hollowed-out face mask, most people’s brains mistakenly convert the image to a face that pops outward off the page. People with schizophrenia, however, are more likely to see the face as it actually is — a concave mask. In that instance, people with schizophrenia give more weight to information that’s coming from their eyes than to their expectation that noses protrude from the rest of the face.
To complicate matters, the opposite can be true, too, says neuropsychologist Chris Frith of the Wellcome Trust Centre for Neuroimaging at University College London. “In this case, their prior is too weak, but in other cases, their prior is too strong,” he says.
In a recent study, healthy people and those who recently began experiencing psychosis, a symptom of schizophrenia, were shown confusing shadowy black-and-white images. Participants then saw color versions of the images that were easier to interpret. When shown the black-and-white images again, people with early psychosis were better at identifying the images, suggesting that they used their prior knowledge — the color pictures — to truly “see” the images. For people without psychosis, the color images weren’t as much help. That difference suggests that the way people with schizophrenia balance past knowledge and present observations is distinct from the behavior of people without the disorder. Sometimes the balance tips too far — in either direction.
In a talk at the annual Computational and Systems Neuroscience meeting in February in Salt Lake City, Seriès described the results of a different visual test: A small group of people with schizophrenia had to describe which way a series of dots were moving on a screen. The dots moved in some directions more frequently than others — a statistical feature that let the scientists see how well people could learn to predict the dots’ directions. The 11 people with schizophrenia seemed just as good at learning which way the dots were likely to move as the 10 people without, Seriès said. In this situation, people with schizophrenia seemed able to learn priors just fine.
But when another trick was added, a split between the two groups emerged. Sometimes, the dots were almost impossible to see, and sometimes, there were no dots at all. People with schizophrenia were less likely to claim that they saw dots when the screen was blank. Perhaps they didn’t hallucinate dots because of the medication they were on, Seriès says. In fact, very early results from unmedicated people with schizophrenia suggest that they actually see dots that aren’t there more than healthy volunteers.
Preliminary results so far on schizophrenia are sparse and occasionally conflicting, Seriès admits. “It’s the beginning,” she says. “We don’t understand much.”
The research is so early that no straightforward story exists yet. But that’s not unexpected. “If 100 years of schizophrenia research have taught us anything, it’s that there’s not going to be a nice, simple explanation,” Adams says. But using math to describe how people perceive the world may lead to new hunches about how that process goes wrong in mental illnesses, he argues.
“You can instill expectations in subjects in many different ways, and you can control what evidence they see,” Adams says. Bayesian theory “tells you what they should conclude from those prior beliefs and that evidence.” If their conclusions diverge from predictions, scientists can take the next step. Brain scans, for instance, may reveal how the wrong answers arise. With a clear description of these differences, he says, “we might be able to measure people’s cognition in a new way, and diagnose their disorders in a new way.”
Now vs. then
The way the brain combines incoming sensory information with existing knowledge may also be different in autism, some researchers argue. In some cases, people with autism might put excess weight on what their senses take in about the world and rely less on their expectations. Old observations fit with this idea. In the 1960s, psychologists had discovered that children with autism were just as good at remembering nonsense sentences (“By is go tree stroke lets”) as meaningful ones (“The fish swims in the pond”). Children without autism struggled to remember the non sequiturs. But the children with autism weren’t thrown by the random string of words, suggesting that their expectations of sentence meaning weren’t as strong as their ability to home in on each word in the series.
Another study supports the notion that sensory information takes priority in people with autism. People with and without autism were asked to judge whether a sight and a sound happened at the same time. They saw a white ring on a screen, and a tone played before, after or at the same time. Adults without autism were influenced by previous trials in which the ring and tone were slightly off. But adults with autism were not swayed by earlier trials, researchers reported in February in Scientific Reports.
This literal perception might get in the way of speech perception, Marco Turi of the University of Pisa in Italy and colleagues suggest. Comprehending speech requires a listener to mentally stitch together sights and sounds that may not arrive at the eyes and ears at the same time. Losing that flexibility could make speech harder to understand.
A different study found that children with autism perceive moving dots more clearly than children without autism (SN Online: 5/5/15). The brains of people with autism seem to prioritize incoming sensory information over expectations about how things ought to work. Elizabeth Pellicano of University College London and David Burr of the University of Western Australia in Perth described the concept in 2012 in an opinion paper in Trends in Cognitive Sciences. Intensely attuned to information streaming in from the senses, people with autism experience the world as “too real,” Pellicano and Perth wrote.
New data, however, caution against a too-simple explanation. In an experiment presented in New York City in April at the annual meeting of the Cognitive Neuroscience Society, 20 adults with and without autism had to quickly hit a certain key on a keyboard when they saw its associated target on a screen. Their job was made easier because the targets came in a certain sequence. All of the participants improved as they learned which keys to expect. But when the sequence changed to a new one, people with autism faltered. This result suggests that they learned prior expectations just fine, but had trouble updating them as conditions changed, said cognitive neuroscientist Owen Parsons of the University of Cambridge.
Distorted calculations — and the altered versions of the world they create — may also play a role in depression and anxiety, some researchers think. While suffering from depression, people may hold on to distorted priors — believing that good things are out of reach, for instance. And people with high anxiety can have trouble making good choices in a volatile environment, neuroscientist Sonia Bishop of the University of California, Berkeley and colleagues reported in 2015 in Nature Neuroscience.
In their experiment, people had to choose a shape, which sometimes came with a shock. People with low anxiety quickly learned to avoid the shock, even when the relationship between shape and shock changed. But people with high anxiety performed worse when those relationships changed, the researchers found. “High-anxious individuals didn’t seem able to adjust their learning to handle how volatile or how stable the environment was,” Bishop says.
Scientists can’t yet say what causes this difficulty adjusting to a new environment in anxious people and in people with autism. It could be that once some rule is learned (a sequence of computer keys, or the link between a shape and a shock), these two groups struggle to update that prior with newer information.
This rigidity might actually contribute to anxiety in the first place, Bishop speculates. “When something unexpected happens that is bad, you wouldn’t know how to respond,” and that floundering “is likely to be a huge source of anxiety and stress.”
Recalculating
“There’s been a lot of frustration with a failure to make progress” on psychiatric disorders, Bishop says. Fitting mathematical theories to the brain may be a way to move forward. Researchers “are very excited about computational psychiatry in general,” she says.
Computational psychiatrist Quentin Huys of the University of Zurich is one of those people. Math can help clarify mental illnesses in a way that existing approaches can’t, he says. In the March issue of Nature Neuroscience, Huys and colleagues argued that math can demystify psychiatric disorders, and that thinking of the brain as a Bayesian number cruncher might lead to a more rigorous understanding of mental illness. Huys says that a computational approach is essential. “We can’t get away without it.” If people with high anxiety perform differently on a perceptual test, then that test could be used to both diagnose people and monitor how well a treatment works, for instance.
Scientists hope that a deeper description of mental illnesses may lead to clearer ways to identify a disorder, chart how well treatments work and even improve therapies. Bishop raises the possibility of developing apps to help people with high anxiety evaluate situations — outsourcing the decision making for people who have trouble. Frith points out that cognitive behavioral therapy could help depressed people recalculate their experiences by putting less weight on negative experiences and perhaps breaking out of cycles of despondence.
Beyond these potential interventions, simply explaining to people how their brains are working might ease distress, Adams says. “If you can give people an explanation that makes sense of some of the experiences they’ve had, that can be a profoundly helpful thing,” he says. “It destigmatizes the experience.”