Editing human germline cells sparks ethics debate
Sci-fi novels and films like Gattaca no longer have a monopoly on genetically engineered humans. Real research scripts about editing the human genome are now appearing in scientific and medical journals. But the reviews are mixed.
In Gattaca, nearly everyone was genetically altered, their DNA adjusted to prevent disease, enhance intelligence and make them look good. Today, only people treated with gene therapy have genetically engineered DNA. But powerful new gene editing tools could expand the scope of DNA alteration, forever changing humans’ genetic destiny.
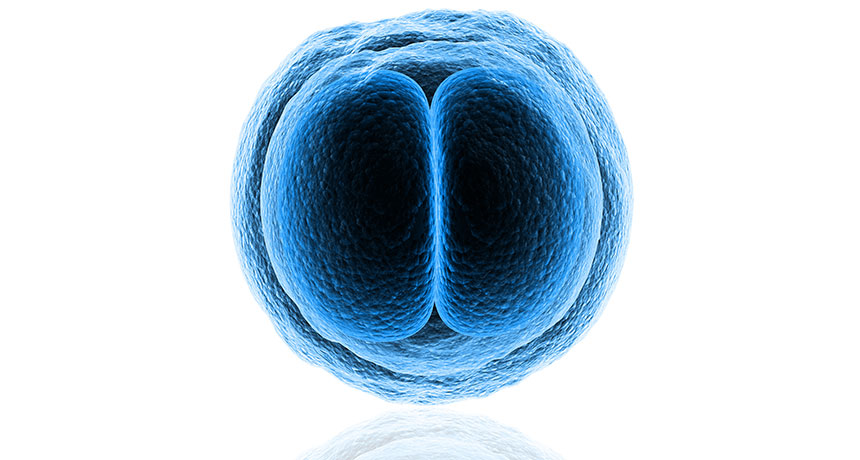
Not everyone thinks scientists should wield that power. Kindling the debate is a report by scientists from Sun Yat-sen University in Guangzhou, China, who have edited a gene in fertilized human eggs, called zygotes. The team used new gene editing technology known as the CRISPR/Cas9 system. That technology can precisely snip out a disease-causing mutation and replace it with healthy DNA. CRISPR/Cas9 has edited DNA in stem cells and cancer cells in humans. Researchers have also deployed the molecules to engineer other animals, including mice and monkeys (SN Online: 3/31/14; SN: 3/8/14, p. 7). But it had never before been used to alter human embryos.
The team’s results, reported April 18 in Protein & Cell, sparked a flurry of headlines because their experiment modified human germline tissue (SN Online: 4/23/15). While most people think it is all right to fix faulty genes in mature body, or somatic, cells, tinkering with the germ line — eggs, sperm or tissues that produce those reproductive cells — crosses an ethical line for many. Germline changes can be passed on to future generations, and critics worry that allowing genetic engineering to correct diseases in germline tissues could pave the way for creating designer babies or other abuses that will persist forever.
“How do you draw a clear, meaningful line between therapy and enhancement?” ponders Marcy Darnovsky, executive director of the Center for Genetics and Society in Berkeley, Calif. About 40 countries ban or restrict such inherited DNA modifications.
Rumors about human germline editing experiments prompted scientists to gather in January in Napa, Calif. Discussions there led two groups to publish recommendations. One group, reporting March 26 in Nature, called for scientists to “agree not to modify the DNA of human reproductive cells,” including the nonviable zygotes used in the Chinese study. A second group, writing in Science April 3, called for a moratorium on the clinical use of human germline engineering, but stopped short of saying the technology shouldn’t be used in research. Those researchers say that while CRISPR technology is still too primitive for safe use in patients, further research is needed to improve it. But those publishing in Nature disagreed.
“Are there ever any therapeutic uses that would demand … modification of the human germ line? We don’t think there are any,” says Edward Lanphier, president of Sangamo BioSciences in Richmond, Calif. “Modifying the germ line is crossing the line that most countries on our planet have said is never appropriate to cross.”
If germline editing is never going to be allowed, there is no reason to conduct research using human embryos or reproductive cells, he says. Sangamo BioSciences is developing gene editing tools for use in somatic cells, an approach that germline editing might render unneeded. Lanphier denies that financial interests play a role in his objection to germline editing.
Other researchers, including Harvard University geneticist George Church, think germline editing may well be the only solution for some people with rare, inherited diseases. “What people want is safety and efficacy,” says Church. “If you ban experiments aimed at improving safety and efficacy, we’ll never get there.”
The zygote experiments certainly demonstrate that CRISPR technology is not ready for daily use yet. The researchers attempted to edit the beta globin, or HBB, gene. Mutations in that gene cause the inherited blood disorder beta-thalassemia. CRISPR/Cas9 molecules were engineered to seek out HBB and cut it where a piece of single-stranded DNA could heal the breach, creating a copy of the gene without mutations. That strategy succeeded in only four of the 86 embryos that the researchers attempted to edit. Those edited embryos contained a mix of cells, some with the gene edited and some without.
In an additional seven embryos, the HBB gene cut was repaired using the nearby HBD gene instead of the single-stranded DNA. The researchers also found that the molecular scissors snipped other genes that the researchers never intended to touch.
“Taken together, our work highlights the pressing need to further improve the fidelity and specificity of the CRISPR/Cas9 platform, a prerequisite for any clinical applications,” the researchers wrote.
The Chinese researchers crossed no ethical lines, Church contends. “They tried to dot i’s and cross t’s on the ethical questions.” The zygotes could not develop into a person, for instance: They had three sets of chromosomes, having been fertilized by two sperm in lab dishes.
Viable or not, germline cells should be off limits, says Darnovsky. She opposes all types of human germline modification, including a procedure approved in the United Kingdom in February for preventing mitochondrial diseases. The U.K. prohibits all other germline editing.
Mitochondria, the power plants that churn out energy in a cell, each carry a circle of DNA containing genes necessary for the organelle’s function. Mothers pass mitochondria on to their offspring through the egg. About one in 5,000 babies worldwide are born with mitochondrial DNA mutations that cause disease, particularly in energy-greedy organs such as the muscles, heart and brain.
Such diseases could be circumvented with a germline editing method known as mitochondrial replacement therapy (SN: 11/17/12, p. 5). In a procedure pioneered by scientists at Oregon Health & Science University, researchers first pluck the nucleus, where the bulk of genetic instructions for making a person are stored, out of the egg of a woman who carries mutant mitochondria. That nucleus is then inserted into a donor egg containing healthy mitochondria. The transfer would produce a person with three parents; most of their genes inherited from the mother and father, with mitochondrial DNA from the anonymous donor. The first babies produced through that technology could be born in the U.K. next year.
Yet another new gene-editing technique could eliminate the need to use donor eggs by specifically destroying only disease-carrying mitochondria, researchers from the Salk Institute for Biological Studies in La Jolla, Calif., reported April 23 in Cell (SN Online: 4/23/15).
Such unproven technologies shouldn’t be attempted when alternatives already exist, Darnovsky says, such as screening embryos created through in vitro fertilization and discarding those likely to develop the disease.
But banning genome-altering technology could leave people with genetic diseases, and society in general, in the lurch, says molecular biologist Matthew Porteus of Stanford University.
“There is no benefit in my mind of having a child born with a devastating genetic disease,” he says.
Alternatives to germline editing come with their own ethical quandaries, he says. Gene testing of embryos may require creating a dozen or more embryos before finding one that doesn’t carry the disease. The rest of the embryos would be destroyed. Many people find that prospect ethically questionable.
But that doesn’t argue for sliding into Gattaca territory, where genetic modification becomes mandatory. “If we get there,” says Porteus, “we’ve really screwed up.”